3-D printing the pre-op plan for PAO
After experiencing years of knee pain, a 22-year-old female collegiate track and field athlete came to Boston Children’s Orthopedic and Sports Medicine Center for treatment. Previous x-rays of her hips showed that she had a combination of hip dysplasia and femoral acetabular impingement (FAI). Her knee pain was likely due to stress on the patella femoral joint caused by running on a malaligned leg with femoral retroversion, as well as pain from the hip injury in the joint presenting as pain in the inner knee.
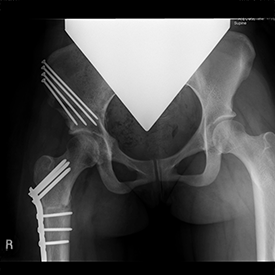
Travis Matheney, MD, MLA, a pediatric hip specialist in the Child and Young Adult Hip Preservation Program at Boston Children’s, developed a staged surgical plan for her treatment. The first surgery would aim to correct her right hip through a right bernese periacetabular osteotomy (PAO), femoral head-neck osteoplasty, and femoral derotational osteotomy.
Through a collaboration with the Boston Children’s Hospital Simulator Program (SIMPeds), a 3-D printed model of the patient’s exact hip and femur was made for the surgical team’s pre-op planning. Although this surgery has been done for years without generating a printed model, this case presented an ideal opportunity to take advantage of the new technology.
By joining the printed femur and hip together, a more accurate determination could be made of whether it was best to fix the hip socket or femur first. The 3-D model also effectively illustrated the lack of rotation in the patient’s femur compared to a normal femur. In addition, when the femur and pelvis models were joined together, it became clear that there was something else happening within the joint.
It was discovered that there was a very subtle extra prominence on the head of the femur. This impingement lesion could have been contributing to the patient’s lack of motion and constant pain.
With this extra information provided by the 3-D model, the decision was made to take a closer look inside the joint during surgery. Once the joint was open, the hip could be manipulated more efficiently, exhibiting how the lesion had been impacting the rim — just like the 3-D model had shown in pre-op. Once the lesion was resected inter-operatively, it created more space within the joint and may ultimately help improve the patient’s motion by 5-10 degrees of rotation and flexion.
Without this 3-D model, it’s unlikely the decision would have been made to open the joint in the first place. Pre-op MRIs showed no significant evidence of a labral tear or cystic changes from chronic injury around the labrum — issues that would typically warrant opening the joint, thus creating the potential for additional scar tissue.
Overall, the procedure went as planned and resulted in a good correction. This first surgery aimed to decrease the impingement that was causing the majority of the patient’s pain and decrease the patient’s risk of early arthritis from the dysplasia. The second stage of surgery will take place next spring to address the same problems with the left hip.
Learn more about the Child and Young Adult Hip Preservation Program at Boston Children’s Hospital Orthopedic and Sports Medicine Center.