Pu Lab | Overview
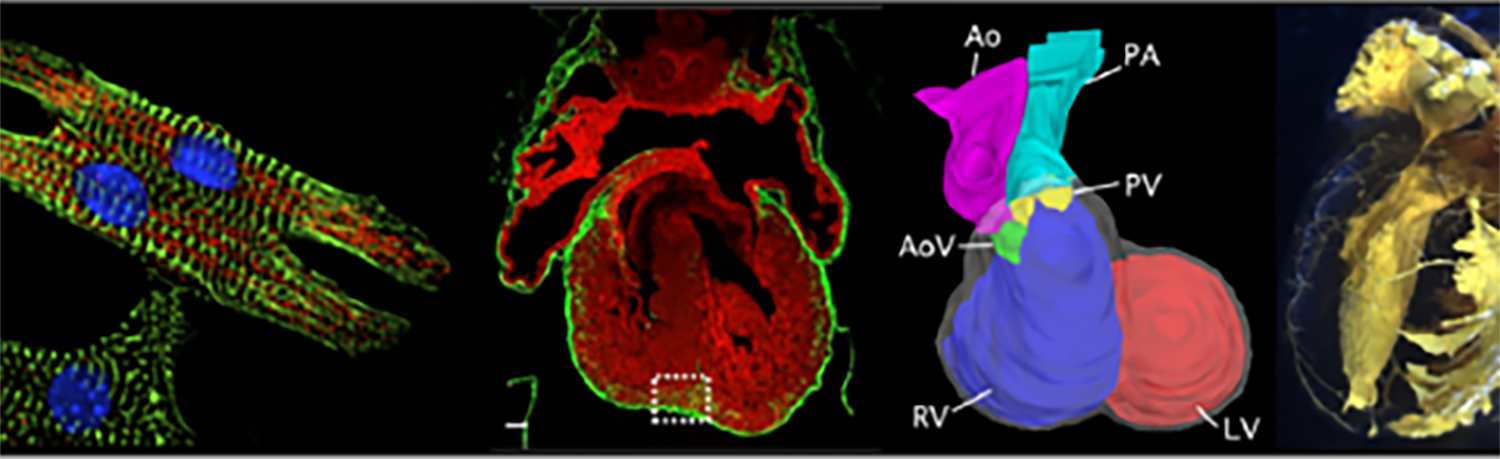
The Pu Lab studies cardiovascular development and disease. We seek to understand fundamental mechanisms that control normal cardiovascular development and function, and how they go awry in cardiovascular disease. Specific areas of interest include:
- Gene regulation in cardiovascular development and disease
- Understanding disease mechanisms in pediatric heart disease
- Development of novel therapies for pediatric heart disease
Gene regulation in cardiovascular development and disease

 The development and function of the heart and vascular system is governed by transcriptional and epigenetic mechanisms, which regulate gene expression. Perturbation of these mechanisms cause congenital heart disease and vascular malformations. The Pu lab is investigating these gene regulatory mechanisms and their abnormalities in cardiovascular disease. To achieve these goals, we are using both genetically engineered mice and induced pluripotent stem cells. We combine genome engineering with CRISPR/Cas9, genome-wide epigenetic and transiptional profiling, single cell RNA-sequencing, and other cutting edge approaches to develop rigorous mechanistic insights.
The development and function of the heart and vascular system is governed by transcriptional and epigenetic mechanisms, which regulate gene expression. Perturbation of these mechanisms cause congenital heart disease and vascular malformations. The Pu lab is investigating these gene regulatory mechanisms and their abnormalities in cardiovascular disease. To achieve these goals, we are using both genetically engineered mice and induced pluripotent stem cells. We combine genome engineering with CRISPR/Cas9, genome-wide epigenetic and transiptional profiling, single cell RNA-sequencing, and other cutting edge approaches to develop rigorous mechanistic insights.
Representative publications:
- He, A., Kong, S. W., Ma, Q. & Pu, W. T. Co-occupancy by multiple cardiac transcription factors identifies transcriptional enhancers active in heart. Proc. Natl. Acad. Sci. U. S. A. 108, 5632–5637 (2011).
- Zhou, P., Gu, F., Zhang, L., Akerberg, B. N., Ma, Q., Li, K., He, A., Lin, Z., Stevens, S. M., Zhou, B. & Pu, W. T. Mapping cell type-specific transcriptional enhancers using high affinity, lineage-specific Ep300 bioChIP-seq. Elife 6, (2017).
- Akerberg BN, Gu F, VanDusen NJ, Zhang X, Dong R, Li K, Zhang B, Zhou B, Sethi I, Ma Q, Wasson L, Wen T, Liu J, Dong K, Conlon FL, Zhou J, Yuan G-C, Zhou P, Pu WT. A reference map of murine cardiac transcription factor chromatin occupancy identifies dynamic and conserved enhancers. Nat Commun. 2019 Oct 28;10(1):4907.
Understanding disease mechanisms in pediatric heart disease
 The lab uses both induced pluripotent stem cells and mice to develop models of heart diseases seen in our Pediatric Cardiology patients. We use these models to develop cellular and molecular insights into disease pathogenesis. These insights allow us to develop novel targeted therapies. Among the diseases we are studying are Barth syndrome, a mitochondrial myopathy, CPVT, an inherited arrhythmia, and Arrhythmogenic Cardiomyopathy, which causes both heart muscle weakness and arrhythmia.
The lab uses both induced pluripotent stem cells and mice to develop models of heart diseases seen in our Pediatric Cardiology patients. We use these models to develop cellular and molecular insights into disease pathogenesis. These insights allow us to develop novel targeted therapies. Among the diseases we are studying are Barth syndrome, a mitochondrial myopathy, CPVT, an inherited arrhythmia, and Arrhythmogenic Cardiomyopathy, which causes both heart muscle weakness and arrhythmia.
Representative publications:
- Wang, G., McCain, M. L., Yang, L., He, A., Pasqualini, F. S., Agarwal, A., Yuan, H., Jiang, D., Zhang, D., Zangi, L., Geva, J., Roberts, A. E., Ma, Q., Ding, J., Chen, J., Wang, D. Z., Li, K., Wang, J., Wanders, R. J., Kulik, W., Vaz, F. M., Laflamme, M. A., Murry, C. E., Chien, K. R., Kelley, R. I., Church, G. M., Parker, K. K. & Pu, W. T. Modeling the mitochondrial cardiomyopathy of Barth syndrome with induced pluripotent stem cell and heart-on-chip technologies. Nat. Med. 20, 616–623 (2014).
- Liu X, Wang S, Guo X, Li Y, Ogurlu R, Lu F, Prondzynski M, de la Serna Buzon S, Ma Q, Zhang D, Wang G, Cotton J, Guo Y, Xiao L, Milan DJ, Xu Y, Schlame M, Bezzerides VJ, Pu WT. Increased ROS-mediated CaMKII activation contributes to calcium handling abnormalities and impaired contraction in Barth syndrome. Circulation. 2021 in press.
- Park S-J, Zhang D, Qi Y, Li Y, Lee KY, Bezzerides VJ, Yang P, Xia S, Kim SL, Liu X, Lu F, Pasqualini FS, Campbell PH, Geva J, Roberts AE, Kleber AG, Abrams DJ, Pu WT*, Parker KK*. Insights Into the Pathogenesis of Catecholaminergic Polymorphic Ventricular Tachycardia From Engineered Human Heart Tissue. Circulation. 2019 Jul 30;140(5):390–404. *co-corresponding
Development of novel therapies for pediatric heart disease
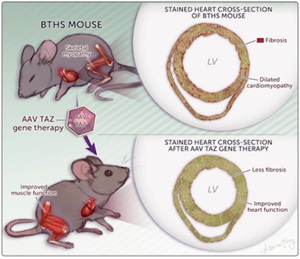 The lab exploits insights into mechanisms underlying inherited heart disease to develop novel therapies. One particularly exciting therapeutic avenue for inherited heart disease is adeno-associated virus (AAV) delivery of therapeutic genetic cargo to heart muscle cells.
The lab exploits insights into mechanisms underlying inherited heart disease to develop novel therapies. One particularly exciting therapeutic avenue for inherited heart disease is adeno-associated virus (AAV) delivery of therapeutic genetic cargo to heart muscle cells.
Representative publications:
- Bezzerides VJ, Caballero A, Wang S, Ai Y, Hylind RJ, Lu F, Heims-Waldron DA, Chambers KD, Zhang D, Abrams DJ, Pu WT. Gene Therapy for Catecholaminergic Polymorphic Ventricular Tachycardia by Inhibition of Ca2+/Calmodulin-Dependent Kinase II. Circulation. 2019 Jul 30;140(5):405–19.
- Wang S, Li Y, Xu Y, Ma Q, Lin Z, Schlame M, Bezzerides VJ, Strathdee D, Pu WT. AAV Gene Therapy Prevents and Reverses Heart Failure in a Murine Knockout Model of Barth Syndrome. Circ Res. 2020 Apr 10;126(8):1024–39.
People
 |
William T. Pu, MDWilliam Pu, MD, is the director of Basic and Translational Cardiovascular Research in the Department of Cardiology at Boston Children’s Hospital, and the Aldo R. Professor of Pediatrics at Harvard Medical School. Dr. Pu has broad expertise in cardiac biology that includes cardiac development, heart failure, cardiac regeneration, and in vitro cardiac disease modeling. His lab has made fundamental discoveries in gene regulation in developing and diseased hearts, particularly in the area of transcriptional regulation. Many of these discoveries are the result of innovative approaches to studying heart development and disease, often involving multidisciplinary collaborations that draw on advances in other fields. His lab is currently engaged in research projects on the genetic causes of inherited heart diseases, and gene therapy for Barth Syndrome and CPVT. Dr. Pu completed his combined BS-MS degree at Yale University and obtained his MD degree from the Harvard Medical School/MIT Science and Technology Program in 1993. He trained in pediatrics and pediatric cardiology at Boston Children’s Hospital. He received his training in basic research in the laboratories of Kevin Struhl, David Clapham, and Seigo Izumo. He established an independent research lab at Boston Children’s in 2004. Contact: wpu@pulab.org
|
News
February 27, 2021
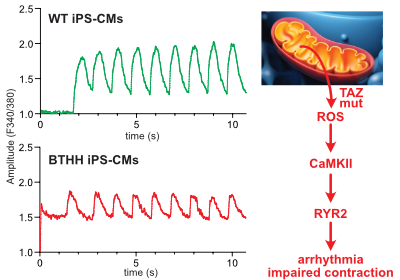
Liu, X. et al., Circulation in press
Barth syndrome cardiomyocytes from human iPSCs and mice have abnormal calcium handling that is partially due to activation of CaMKII. Barth syndrome mice had increased vulnerability to arrhythmia, perhaps reflecting the abnormal calcium handling.
January 20, 2021
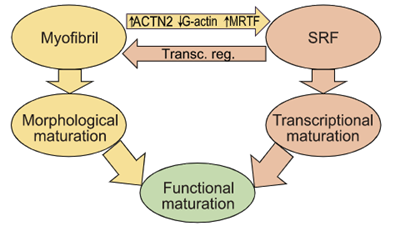
Guo, Cao et. al. PNAS - Read the article
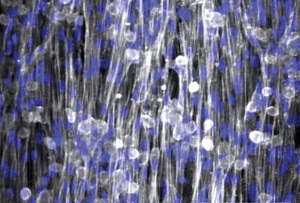
Sarcomere assembly promotes MRTF-SRF signaling to drive a feed-forward circuit that stimulates cardiomyocyte maturation.
March 10, 2020

Wang, S et al., Circ. Res. In press. Read the article
AAV gene therapy improved survival and heart and skeletal muscle function in a new mouse model of Barth syndrome.
March 5, 2020
In press in Circulation Research.
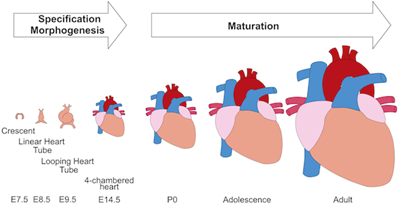
Cardiomyocyte maturation is the process whereby proliferative and glycolytic fetal cardiomyocytes become specialized to forcefully and efficiently contract billions of times in an animal’s lifespan. This review article by Yuxuan Guo and William Pu summarizes our current understanding of mechanisms that promote and coordinate the process of cardiomyocyte maturation.
October 29, 2019
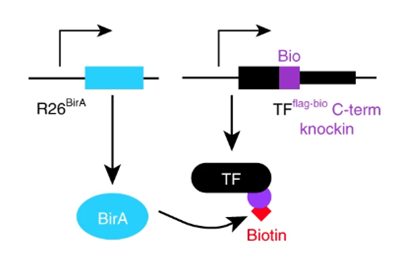
Mapping transcription factors (TFs) occupancy is essential for understanding transcriptional programs. Here Akerberg, Gu, and colleagues use biotinylated knockin alleles of key cardiac TFs (GATA4, NKX2-5, MEF2A, MEF2C, SRF, TBX5, TEAD1) to map their genome-wide occupancy in the fetal and adult mouse heart, providing insight into the cardiac transcriptional regulatory network.
July 21, 2019
In an equal collaboration between the Pu and Parker labs, Park, Zhang, et al. describe development of an engineered human tissue model of CPVT. Using this model, the investigators dissected the molecular pathway linking exercise to unmasking of the arrhythmia mutation. The study revealed that CaMKII phosphorylation of RYR2-S2814 is essential for expression of multiple RYR2 mutations.
Background:
Modeling of human arrhythmias using induced pluripotent stem cell-derived cardiomyocytes has focused on single cell phenotypes. However, arrhythmias are the emergent properties of cells assembled into tissues, and the impact of inherited arrhythmia mutations on tissue-level properties of human heart tissue has not been reported.
Methods:
Here, we report an optogenetically-based, human engineered tissue model of catecholaminergic polymorphic ventricular tachycardia (CPVT), an inherited arrhythmia caused by mutation of the cardiac ryanodine channel (RYR2) and triggered by exercise. We developed a hiPSC-CM-based platform to study the tissue-level properties of engineered human myocardium. We investigated pathogenic mechanisms in CPVT, by combining this novel platform with genome editing.
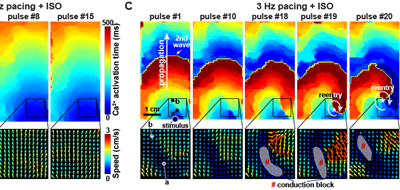
Results:
In our model, CPVT tissues were vulnerable to develop reentrant rhythms when stimulated by rapid pacing and catecholamine, recapitulating hallmark features of the disease. These conditions elevated diastolic Ca2+ levels and increased temporal and spatial dispersion of Ca2+ wave speed, creating a vulnerable arrhythmia substrate. Using Cas9 genome editing, we pinpointed a single catecholamine-driven phosphorylation event, RYR2-S2814 phosphorylation by Ca2+-calmodulin-dependent protein kinase II (CaMKII), that is required to unmask the arrhythmic potential of CPVT tissues.
Conclusions:
Our study illuminates the molecular and cellular pathogenesis of CPVT and reveals a critical role of CaMKII-dependent reentry in the tissue-scale mechanism of this disease. We anticipate that this approach will be useful to model other inherited and acquired cardiac arrhythmias.
June 23, 2019
Background:
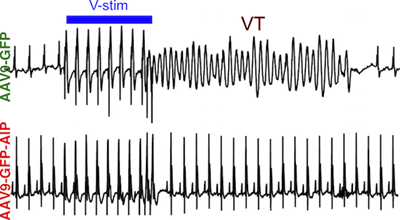
Catecholaminergic polymorphic ventricular tachycardia (CPVT), an inherited cardiac arrhythmia characterized by adrenergically triggered arrhythmias, is inadequately treated by current standard of care. Ca2+/calmodulin-dependent protein kinase II (CaMKII), an adrenergically activated kinase that contributes to arrhythmogenesis in heart disease models, is a candidate therapeutic target in CPVT. However, translation of CaMKII inhibition has been limited by the need for selective CaMKII inhibition in cardiomyocytes. Here we tested the hypothesis that CaMKII inhibition using a cardiomyocyte-targeted gene therapy strategy would suppress arrhythmia in CPVT mouse models.
Methods:
We developed AAV9-GFP-AIP, an adeno-associated viral vector in which a potent CaMKII inhibitory peptide (AIP), is fused to GFP and expressed from a cardiomyocyte selective promoter. The vector was delivered systemically. Arrhythmia burden was evaluated using invasive electrophysiology testing in adult mice. AIP was also tested on induced pluripotent stem cells (iPSC) derived from CPVT patients with different disease-causing mutations to determine the effectiveness of our proposed therapy on human iPSC-derived cardiomyocytes (iPSC-CMs) and different pathogenic genotypes.
Results:
AAV9-GFP-AIP was robustly expressed in the heart without significant expression in extra-cardiac tissues, including the brain. Administration of AAV9-GFP-AIP to neonatal mice with a known CPVT mutation ( RYR2R176Q/+) effectively suppressed ventricular arrhythmias induced by either β-adrenergic stimulation or programmed ventricular pacing, without significant proarrhythmic effect. Intravascular delivery of AAV9-GFP-AIP to adolescent mice transduced ~50% of cardiomyocytes and was effective in suppressing arrhythmia in CPVT mice. iPSC-CMs derived from two different CPVT patients with different pathogenic mutations demonstrated increased frequency of abnormal calcium release events, which was suppressed by a cell-permeable form of AIP.
Conclusions:
This proof-of-concept study showed that AAV-mediated delivery of a CaMKII peptide inhibitor to the heart was effective in suppressing arrhythmias in a murine model of CPVT. CaMKII inhibition also reversed the arrhythmia phenotype in human CPVT iPSC-CMs models with different pathogenic mutations.
Get involved
We are always looking for creative, motivated, and productive postdoctoral fellows and research assistants. Please send CV and 3 letters of recommendation to Dr. Pu at wpu@pulab.org.
