Heterotaxy | Symptoms & Causes
What are the symptoms of heterotaxy syndrome?
The symptoms of heterotaxy syndrome vary depending on the complexity of heart disease and the involvement of other organs.
Heart symptoms may include:
- cyanosis (blue skin, usually on the lips and under the fingernails)
- labored or fast breathing
- abnormally slow or fast heart rate
- difficulty feeding
- poor weight gain
Gastrointestinal (GI) tract symptoms may include:
- difficulty feeding
- frequent vomiting
- bilious (dark green) vomiting
Weakened immunity symptoms may include:
- frequent infections
Lung and airway symptoms may include:
- frequent infections
- difficulty clearing mucus from the lungs
What are the causes of heterotaxy syndrome?
Heterotaxy syndrome is caused by genetic abnormalities. These abnormalities may be inherited from one or both parents, or they randomly happen. For some children, blood tests can detect a specific gene that may cause heterotaxy, but in many others, a genetic cause can’t be identified.
A positive genetic testing result can help understand a child’s prognosis and risk for complications outside of their heart. It can also be used to understand if other family members are at risk for having the condition and the likelihood that the parents of a child with heterotaxy could have a second affected child.

Check out our downloadable pamphlet for a summary about heterotaxy syndrome. It provides details about the diagnosis, testing, treatment at Boston Children’s, and more.
Common issues with heterotaxy syndrome
Congenital heart defects, often involving a combination of the following:
- an abnormal heart position, such as dextrocardia (right-sided heart) or mesocardia (heart in the middle of the chest)
- holes in the walls that divide the right and left sides of the heart, including an atrial septal defect, ventricular septal defect, or atrioventricular canal defect (sometimes called atrioventricular septal defect)
- abnormal blood vessel positions, such as transposition of the great arteries (TGA)
- blockage of blood flow to the lungs (pulmonary valve stenosis) or to the body (aortic valve stenosis or coarctation of the aorta)
- underdeveloped pumping chambers (single ventricle defects)
- abnormally connected veins (interrupted inferior vena cava or total anomalous pulmonary venous return)
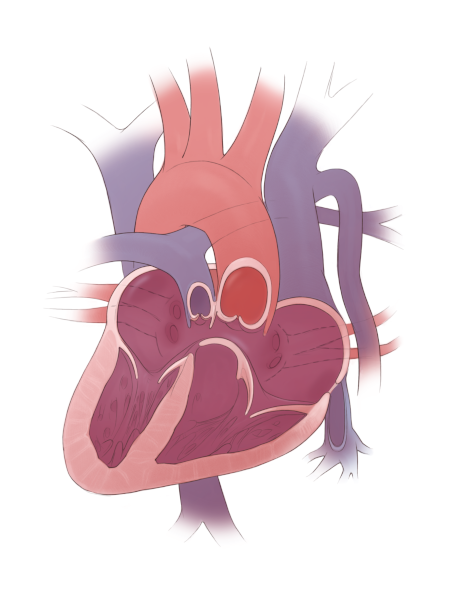
Heterotaxy heart with dextrocardia, complete atrioventricular canal defect, double outlet right ventricle, pulmonary stenosis, and interrupted inferior vena cava
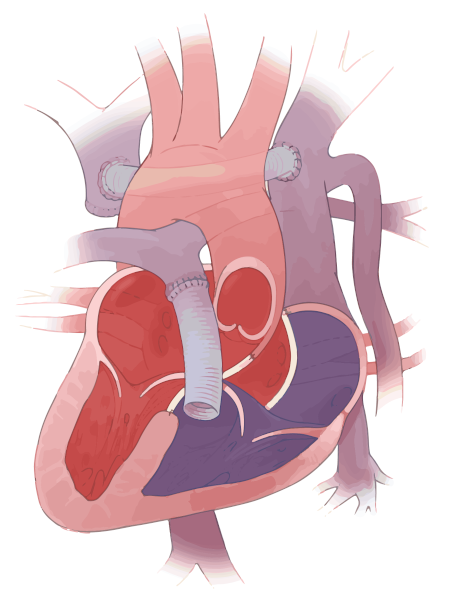
Heterotaxy heart after complete biventricular repair including repair of the atrioventricular canal defect, right ventricle-to-pulmonary artery conduit, and creation of a neo-innominate vein
Heart rhythm:
- slow heart rhythm (heart block)
- fast heart rhythm (supraventricular tachycardia)
- abnormal heart rhythm pathways (dual atrioventricular nodes)
Lungs and airways:
- structural problems in the lungs
- primary ciliary dyskinesia (PCD), a lung condition in which cilia, the tiny hair-like cells that line the respiratory tract, are not formed the right way or may not work properly. This can cause chronic nasal or chest congestion, pneumonia, and abnormal dilation of the airway (bronchiectasis)
Immune system:
- having no spleen (asplenia) or many small spleens (polysplenia) that may not work properly
- increased risk of infection
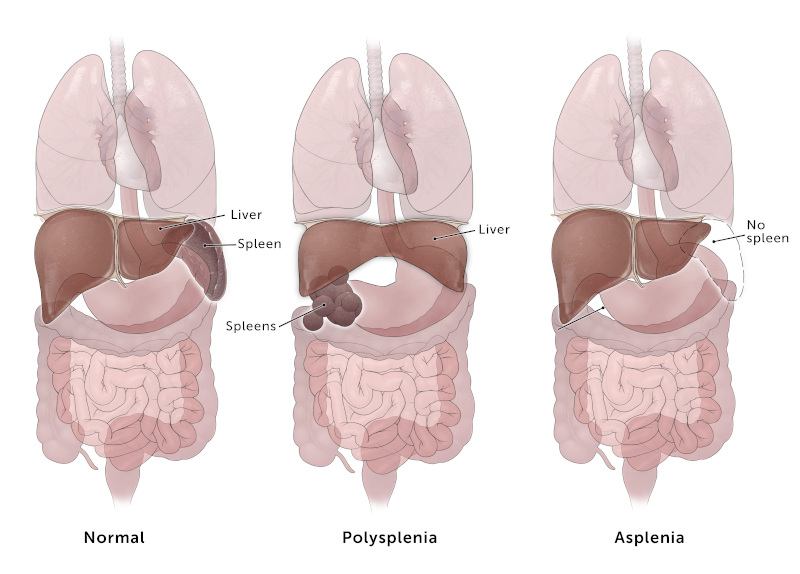
How the spleen can be affected by heterotaxy
The spleen is often affected in children with heterotaxy, which increases risk of infection. Read more about heterotaxy and your child's immune system.
GI tract:
- abnormal arrangement of the intestines (malrotation or nonrotation)
- a liver that is in the wrong location
- bile system abnormalities (biliary atresia)
- abnormal liver blood flow (Abernethy syndrome)
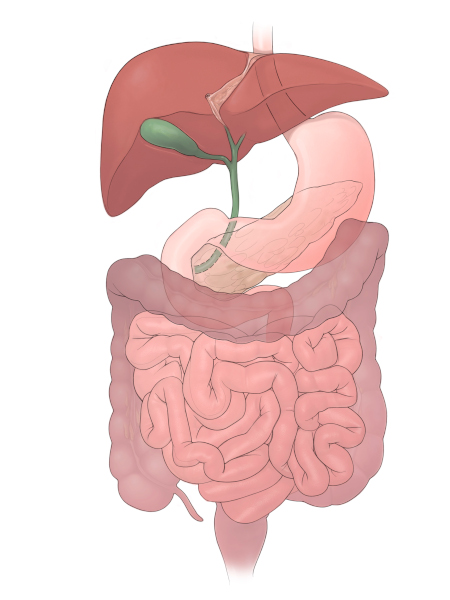
Normal abdominal anatomy
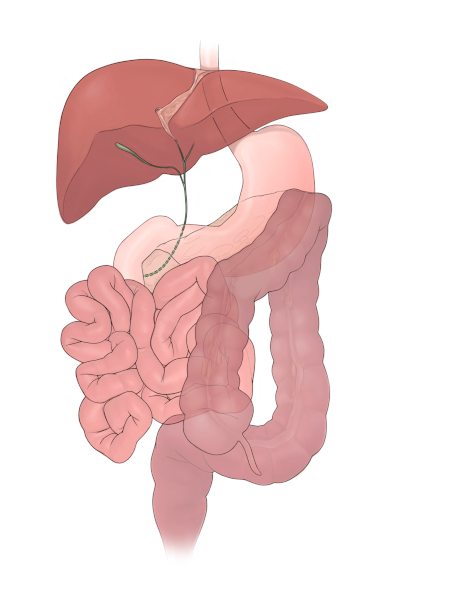
Intestinal malrotation and biliary atresia
Heterotaxy | Diagnosis & Treatments
How is heterotaxy syndrome diagnosed?
Heterotaxy syndrome is diagnosed many different ways. It is often diagnosed before birth, when an ultrasound identifies an abnormal position of one or more organs. Sometimes, it can be diagnosed with a fetal echocardiogram (a special ultrasound of the heart before birth) when a complex heart defect is identified. Also, heterotaxy may be diagnosed during infancy or childhood if your child has feeding problems, breathing problems, cyanosis (blue color), a heart rhythm issue, or a heart murmur.
If heterotaxy syndrome is suspected, your medical team may use the following tests to get a complete picture of your child’s heart and anatomy:
- chest x-ray, to get an overview of the size and position of the heart and the lungs
- electrocardiogram (ECG or EKG), to get an overview of the heart rhythm
- holter monitor, a 24-hour test to get extensive heart rhythm information
- echocardiogram, an ultrasound that shows the structure and function of the heart
- cardiac magnetic resonance imaging (MRI) or computed tomography (CT), which are advanced diagnostic tests to show additional details of the heart
- cardiac catheterization, to check pressures in different areas of the heart
Your child might be screened for other potential health concerns that could be associated with heterotaxy and may need these tests:
- abdominal/liver ultrasound
- lung tests such as a nasal ciliary swab and nasal nitric oxide measurements
- spleen scan
- genetic testing
How is heterotaxy syndrome treated?
Children with heterotaxy syndrome require lifelong follow-up care. The care that your child needs will depend on which systems within the body are affected and the severity. Some children with heterotaxy syndrome who have severe heart defects may need heart surgery shortly after birth to stabilize their circulation. Other children are only mildly affected and may never need surgery.
Children with abnormal cilia may need special inhaled medications to keep their lungs healthy. Those with immune system problems may need daily antibiotic treatment and extra vaccinations to prevent certain infections. Children with malrotation who develop an intestinal blockage may need corrective surgery. Your child’s care team will review test results with you and then develop a treatment plan that is best for your child.

A biventricular repair helps California girl thrive
Born with heterotaxy, Elyse had three surgeries in California before coming to Boston Children's for a second opinion and biventricular repair.
How we care for heterotaxy syndrome
Heterotaxy syndrome can be very complex, and every child’s needs are different. The Heterotaxy Program at Boston Children’s takes a comprehensive approach to treating children with heterotaxy syndrome. We bring together specialists from several disciplines who have extensive experience treating the many conditions associated with heterotaxy.
We screen for and identify potential problems associated with the condition, and collectively create an individualized treatment plan that best addresses the specific complexities of your child’s case. We work together to find treatment solutions for even the most challenging cases. For instance, children with complex heart defects who were previously thought to be candidates for only single-ventricle palliation, or who have already had single-ventricle palliation procedures such as Glenn or Fontan surgeries at other hospitals, might qualify for “two-ventricle” (biventricular) repairs. No matter the type of condition, we will work together to provide a lifetime of care for your child.


