Bladder Exstrophy and Epispadias | Symptoms & Causes
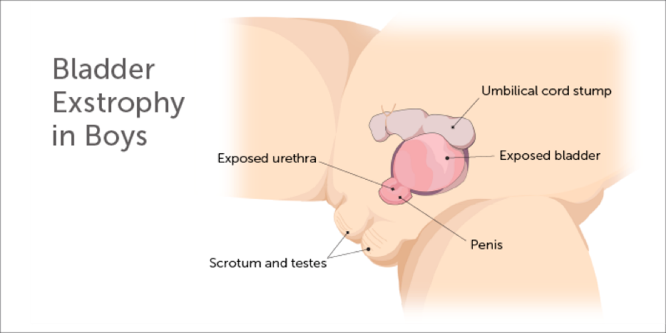
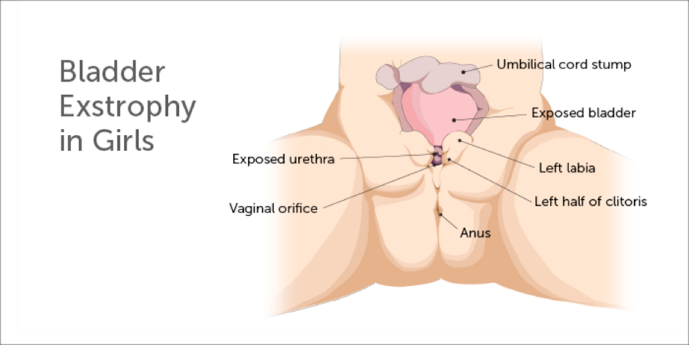
What causes bladder exstrophy and epispadias?
The cause of bladder exstrophy and epispadias is unknown. Popular theories suggest a normal structure known as the cloacal membrane might overdevelop in these babies. That might prevent appropriate tissue development, ingrowth, and the joining together of the supportive lower abdominal wall structure. Some studies show a clustering of the condition in families, suggesting that there’s an inherited factor. However, the chance for parents to have another child with exstrophy of the bladder is less than 1 percent.
Bladder Exstrophy and Epispadias | Diagnosis & Treatments
How is bladder exstrophy diagnosed?
Bladder exstrophy may be diagnosed during a routine fetal ultrasound or other indicated imaging techniques such as magnetic resonance imaging (MRI). Often it is diagnosed immediately after birth during initial physical examination.
Prenatal care is an important aspect of health for every expectant mother and fetus. The prenatal diagnosis of bladder exstrophy allows time for learning about the condition and preparing for the anticipated care.
How is bladder exstrophy treated?
Treatment for bladder exstrophy begins at birth. Your care team should be readily available to help you in the immediate post-natal period. The primary goal when caring for a child with bladder exstrophy is to:
- preserve normal kidney function
- develop adequate bladder function and promote urinary continence
- provide acceptable appearance and function of the external genitalia
- ensure that your child has a typical and normal childhood
Bladder exstrophy repair
Complete primary repair of bladder exstrophy (CPRE)
CPRE is a procedure in which the bladder is closed, the bladder neck (area of transition from bladder to urethra) is reconstructed, and the epispadias is repaired (entire urethra is closed into a tube) at the same time. Incisions in the pelvic bones (osteotomies) are performed at the time of CPRE in order to help provide more normal anatomy of the bones and muscles of the pelvis. Children who undergo CPRE will may require additional surgery during later years to manage urinary incontinence and vesicoureteral reflux (VUR).
This initial reconstruction (CPRE) is usually performed at approximately 6 to 8 weeks of life. Delaying CPRE beyond the first 2 to 3 days of life may have several advantages for the child. This timing presents an opportunity for normal bonding between the baby and parents before the initial reconstructive surgery and lengthy recovery period that follows. The time between birth and initial repair allows for growth, development, and additional maturation of some organs and systems prior to the complex surgery and makes the anesthesia and surgery safer.
At Boston Children’s, we prefer CPRE for initial reconstruction of babies with bladder exstrophy for several reasons. These include earlier bladder cycling (filling and emptying) compared to staged approach, and potentially obtaining all of the benefits of a staged approach in one single operation. Following CPRE, your baby is kept safe in a spica cast for approximately eight weeks in order to optimize safety and healing. However, they may leave the hospital as early as seven to 10 days after the surgery.
Modern staged repair of bladder exstrophy (MSRE)
Although CPRE is our preferred technique we have experience in the MSRE approach as well. MSRE involves three surgeries for reconstruction of bladder exstrophy:
- The initial repair (bladder closure): The bladder and abdominal wall are closed, the belly button is reconstructed, and an osteotomy is sometimes performed (the pelvic bones are reformed to aid in the repair). The initial repair is usually performed in the first 2 to 3 days of life.
- The second stage (epispadias repair): In boys, the proximal part of the urethra close to the bladder is closed along with the bladder. In girls, the urethra is usually closed along its entire length, extending all the way from the bladder to the surface of the skin between the labia as it normally should be. The second stage repair occurs around 6 to 12 months of age.
- The third stage (bladder neck reconstruction): This stage involves bladder neck reconstruction with bilateral ureteral reimplantation. This stage is performed when the bladder has grown sufficiently to hold an appropriate volume of urine. This procedure is usually performed between the ages of 6 to 10 years of age.
What is the long-term outlook for bladder exstrophy?
After their initial treatment for bladder exstrophy, your child will require lifelong follow-up. Care is ongoing and can involve a range of testing to evaluate your child’s growth and development, ensure kidney health, and, in some instances, determine the need for physical therapy, medication, or an additional surgical procedure. In some cases, additional surgery is required during childhood, adolescence, and young adulthood.
Boston Children’s is committed to providing the care that your child needs. Every child is different, and as your child grows, their bladder and kidneys grow with them. Our doctors and nurses in the Bladder Exstrophy Program will work with you to develop the best plan of care specific to your child’s needs all along the way.
How we care for bladder exstrophy and epispadias
The experts in our Bladder Exstrophy Program are dedicated to providing exceptional pediatric care. Our team includes physician specialists in urology, nephrology, orthopedic surgery, anesthesiology, radiology, and nuclear medicine, as well as nurses, social workers, and child life specialists who will care and support you and your child at every step, from diagnosis through treatment, and even after your child returns home. We are always here to answer any questions and to listen to your concerns.
We offer a variety of resources for families, including access to the Fetal Care and Surgery Center (MFCC). The MFCC provides support through prenatal counseling, treatment, and follow-up for families with a confirmed or suspected fetal congenital anomaly. In addition, medical staff, social workers, child life specialists, and spiritual care services are available to support the expectant mother and her family.